12 Mar Qualifying & Paying for Medicare Part A
We are often asked about how to qualify for Medicare, so we thought that we would share information about the four parts to Medicarecoverage. Today, we’ll be covering how to qualify for Medicare Part A and ways to access premium-free Medicare Part A coverage.
What is Medicare Part A?
Medicare Part A covers medical care that you received will hospitalized, as well as some types of health care. According to Medicare.gov, Part A generally covers:
- Inpatient care in a hospital
- Skilled nursing facility care
- Inpatient care in a skilled nursing facility (not custodial or long-term care)
- Hospice care
- Home health care
How do I qualify for Medicare Part A?
Most people are automatically eligible for Medicare Part A at age 65, if they’re eligible for retirement benefits from the Social Security Administration or the Railroad Retirement Board.
You may qualify for Medicare Part A before the age of 65, if you have received Social Security Disability Insurance (SSDI) benefits for two years, have end-stage renal disease (ESRD), or have amyotrophic lateral sclerosis (ALS).
In order to receive Medicare, you must also be either a United States citizen or a legal permanent resident for at least five continuous years.
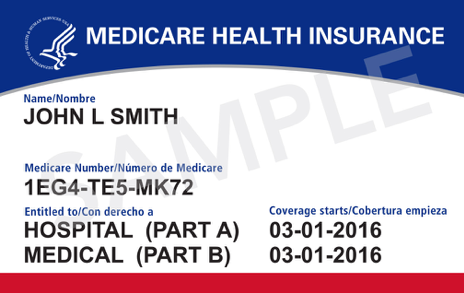
Most people do not pay a monthly premium for Medicare Part A, as long as they have worked at least 10 years (or 40 quarters) and paid Medicare taxes during that time. Individuals who aren’t eligible for premium-free Medicare Part A because they have not worked enough quarters, can still enroll in Part A, but they will have to pay a monthly premium.
| Number of quarters that you worked and paid Medicare taxes | Monthly Premium Amount |
| 40+ quarters | $0 |
| 30-39 quarters | $232 |
| Less than 30 quarters | $422 |
How do I enroll in Medicare Part A?
When you first become eligible for Medicare (e.g., you are turning 65), enrollment in Medicare Part A is usually automatic. Medicare Part A benefits begin the first day of the month you turn 65. If your birthday is on the first day of the month, your benefits will begin the month before you turn 65. You also have an Initial Enrollment Period, during the three months before you turn 65, the month you turn 65, and three months after you turn 65. You can make additional decisions about your Medicare coverage (other than Part A) during this time.
It is critical not to miss your initial enrollment period, because individuals who delay enrollment after they first become eligible for Medicare Part A may be subject to late enrollment penalties once they sign up.
If you did delay enrolling in Medicare Part A, you may still enroll, but you will have to wait until the next available General Enrollment Period. The General Enrollment Period occurs each year from January 1 to March 31. If you sign up during general enrollment, your coverage will begin July 1 of that year.
You may also be eligible for a special enrollment period. If you (or your spouse) lose your employer-sponsored health insurance, or if you were a volunteer serving in a foreign country, you may enroll in Medicare Part A immediately or during a Special Enrollment Period (SEP). This is the eight-month period that begins the month after your employment or other group coverage ends (whichever happens first).
The Qualified Medicare Beneficiary program (QMB)
Premium-free Part A Medicare may still be available to low-income individuals who do not have enough work quarters through the Qualified Medicare Beneficiary program (QMB).
Under the QMB benefit, state Medicaid programs pay for the Part A and Part B premiums. QMBs also get assistance paying for Medicare deductibles and co-insurance payments. The QMB program is generally available to people with incomes at or below 100% of the Federal Poverty Level with limited assets.
Individuals in most states (Part A “buy-in” states) can apply for conditional Part A at any time of the year. With proof of conditional application, they can then immediately apply for the QMB program with their state Medicaid program.
However, in 14 states (Part A “Group Payer” states) SSA can only accept conditional Part A applications during the General Enrollment Period (January 1-March 31) and coverage would begin July 1. The Group Payer states are Alabama, Arizona, California, Colorado, Illinois, Kansas, Kentucky, Missouri, Nebraska, New Jersey, New Mexico, South Carolina, Utah and Virginia.
Looking for additional information?
For more resources and help:
- Watch our webinar on Medicare
- Visit Medicare.gov
- Read our blog on Medicare’s Extra Help Program


